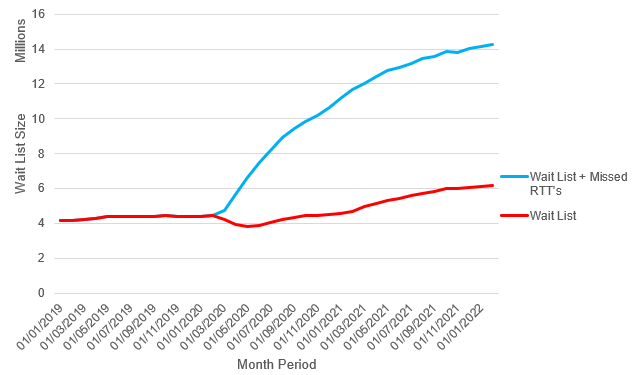
As the NHS’s known waiting list soars to record highs of 6,183,203 in England alone, with some individuals waiting for over 2 years for treatment for the first time in history, it is abundantly clear that this is a very real problem effecting millions of those who call this country home. Unfortunately, as my last post highlighted, this doesn’t paint the whole picture. Analysis I have been working on has been investigating how many referral to treatment’s have been missed during the Covid-19 period.
A Referral To Treatment (RTT) occurs when it is decided an individual needs to see a consultant, usually by a primary care practitioner such as a GP. These are for conditions that will not self resolve, in other words each and every RTT is for a condition someone has that will not go away on it’s own. This explains why an RTT that should have happened a year ago is still a problem as it is likely still effecting that individual and if anything, worsening.
Analysis shows that up to February 2022, there are over 8,000,000 missed RTT’s, more than doubling the waiting list the NHS currently knows.
Methodology
Firstly, to analyse the Covid-19 period we had to find a ‘baseline’ number of new RTT’s to compare to. This was chosen to be the year prior to the impact Covid had in the UK, March 2019 to February 2020. For months in this period, a 3 month centred smoothed average was used, except for the first and last months (March 2019, and February 2020) where a left and right window had to be used. Once these averages were calculated, the number of RTT’s in each month during the Covid period was subtracted from it’s respective month in the baseline. Positive numbers represented missed RTT’s, and negative would indicate that more RTT’s than expected occurred during that month.
This method was carried out for every CCG (Clinical Commissioning Group) in England and the total number of missed RTT’s was found by summing the total across all of the CCG’s. Sometimes, CCG’s merged to create a larger CCG, when this occurred these mergers were retrospectively applied to the beginning of the analysis period to ensure parity in the populations these RTT’s were occurring in during the Covid period. Stratifying this analysis by CCG allowed for regional differences to be identified (which I may discuss in a future post), as well as potentially identifying what allowed certain CCG’s to perform well.
References/Publications:
LCP Report – Hidden health needs – the elephant in the NHS waiting room
NHS RTT’s – Consultant-led Referral to Treatment Waiting Times